Ask an Expert: All About Hypotonia with Dr. Maral Amani, PT, DPT
May 26, 2025
Dr. Maral Amani, PT, DPT, is a licensed pediatric doctor of physical therapy and mom, who is certified in early intervention (children 0-3 years old). She is a play-based therapist who is passionate about supporting children with disabilities, delays, and neurodivergence through family-centered care. She educates parents and caregivers through her work as an in-home therapist across San Diego and on her Instagram.

Finding out that your baby has hypotonia can bring up many emotions, questions, and feelings of uncertainty. Because a hypotonia diagnosis means that your little one has decreased muscle tone, it can affect their gross motor development. With physical therapy and other treatments, however, your child can build stronger muscles over time. Here’s everything you need to know about hypotonia.
What is hypotonia?
Muscle tone refers to the amount of tension or resistance to movement in a muscle when it is at rest. There is a wide range of typical muscle tone across individuals. Hypotonia, often described as "low muscle tone," occurs when resting muscle tension is lower than what is considered typical. It is the opposite of hypertonia, or increased muscle tone.
What causes hypotonia?
Hypotonia is most often a symptom of an underlying condition and is commonly present from birth. However, some children may receive a diagnosis of benign congenital hypotonia when no specific cause is identified. Conditions frequently associated with hypotonia include Down syndrome, prematurity, autism spectrum disorder, Williams syndrome, and spinal muscular atrophy. Hypotonia is not preventable, and is often related to genetic, neurological, or developmental conditions that occur during pregnancy or early development.
What are the symptoms of hypotonia and how is it diagnosed?
Hypotonia isn't always immediately obvious, but it is often identified due to delayed milestones. The first milestone of head control is often delayed, which can cause a pediatrician to recommend an assessment by a pediatric physical therapist. Parents may notice their baby feels unusually “floppy” or seems to slip through their hands when lifted. Hypotonia can affect the whole body or be more localized, such as in the facial or oral muscles. For example, a baby with low oral tone may rest with their mouth open.

How does hypotonia affect gross motor milestones?
Children with hypotonia can reach all of their gross motor milestones—although they may achieve them later and with more effort. Because their muscles require more energy to activate, activities like squatting or crawling may fatigue them more quickly. As a result, they may need more practice, support, and rest breaks compared to peers.
What can I expect after a hypotonia diagnosis?
After a hypotonia diagnosis, your child will likely be referred to a pediatric physical therapist. If motor delays are present, such as difficulty with head control, rolling, or crawling, therapy will target the muscles and movement patterns involved in those skills. For example, if your baby struggles with head control, therapy will include activities to strengthen the neck and trunk muscles.
Can hypotonia be outgrown?
Muscle tone is a neurological characteristic (regulated by nerve impulses originating in the brain that reach the whole body through motor nerves) and typically does not change over time. However, children with hypotonia can build strength and coordination through targeted physical activity. While low tone remains, improved muscle strength can reduce its functional impact on development.
What does tummy time look like with hypotonia?
An infant with hypotonia may struggle to lift and maintain their head during tummy time, due to decreased muscle activation. They often need more frequent, shorter sessions to build endurance and strength gradually. Consistent practice, even in brief bursts, is key to progress.

How is hypotonia treated?
Hypotonia can affect both large (gross motor) and small (fine and oral motor) muscles, potentially leading to delays in movement, coordination, speech, or feeding. If left untreated, these delays may build upon each other and impact a child’s overall development. Early intervention through physical and occupational therapy can significantly improve outcomes.
The duration of physical therapy varies based on the underlying diagnosis and how significantly hypotonia affects development. Some children, such as those with Down syndrome, may benefit from therapy throughout childhood in phases. Others, like infants born prematurely, may only need therapy for a limited time. Each child’s needs are unique, and therapy plans are tailored accordingly.
Shop the blog
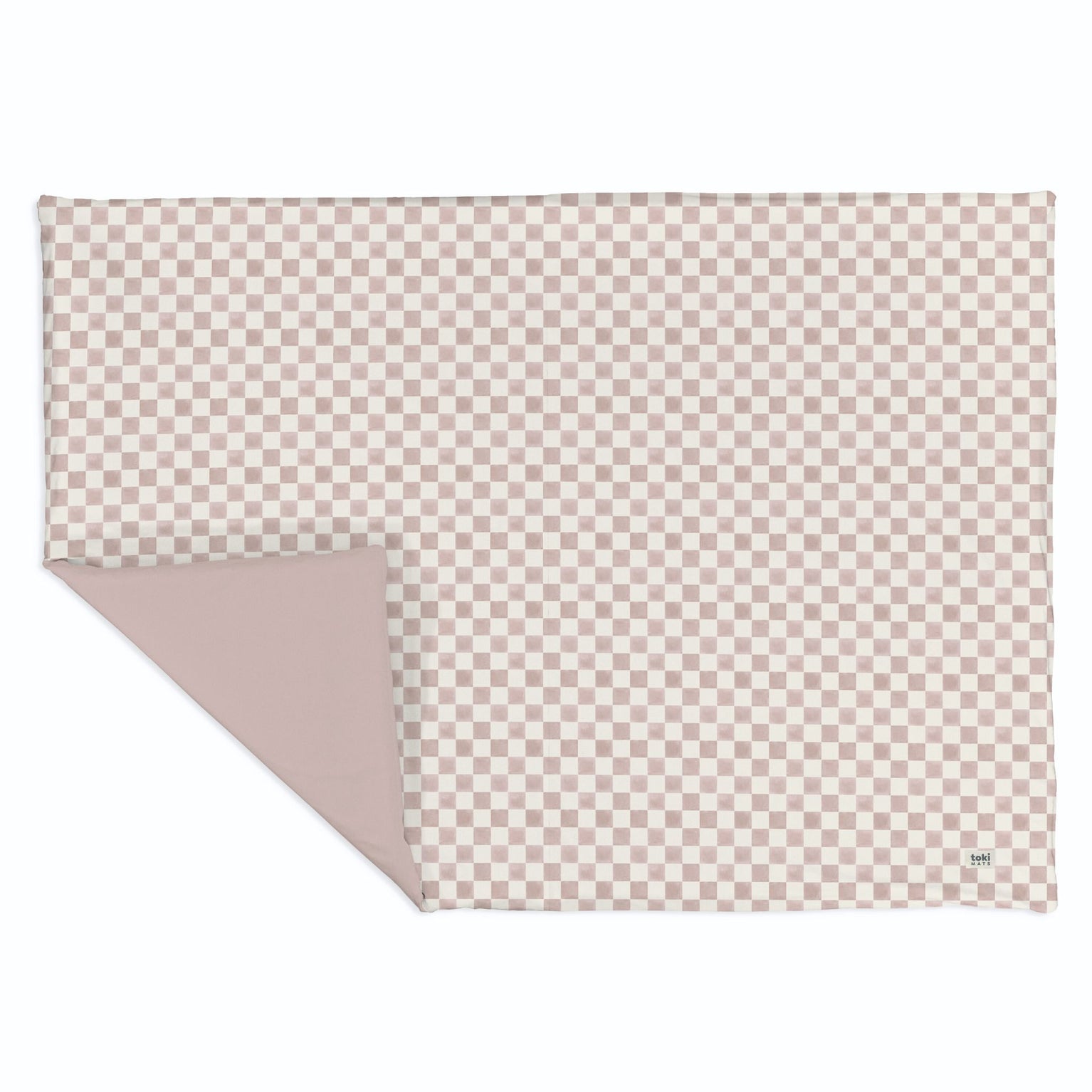
Checker Gumdrop Organic Cotton Mat
$455 - $455
Meet the super comfy, easy-to-clean play mat of your dreams! Made for tummy time, play time, and life on the go.

About the Author: Alice
Alice Mendoza is a copywriter and blog writer based in Los Angeles. She began writing for a baby brand while on maternity leave, and realized she had found her niche. Today, she writes exclusively within the baby space, using her BFA in Creative Writing and her own experience as a mother to guide her. When she’s not working, you can find her chasing down her toddler, going on walks around the neighborhood, or watching reality TV.


































